This blog post is my/Dave’s experience with Haglund’s Deformity and should not be considered medical advice. If you have Haglund’s Deformity, consult your physician, and understand that your journey will be separate from mine.
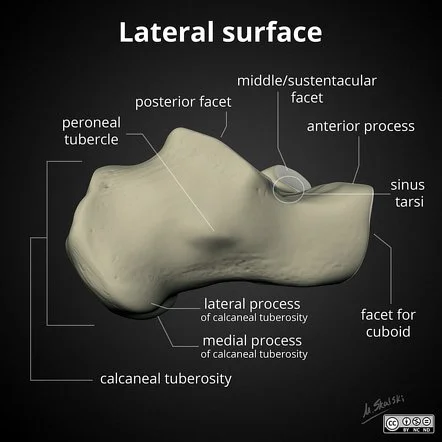
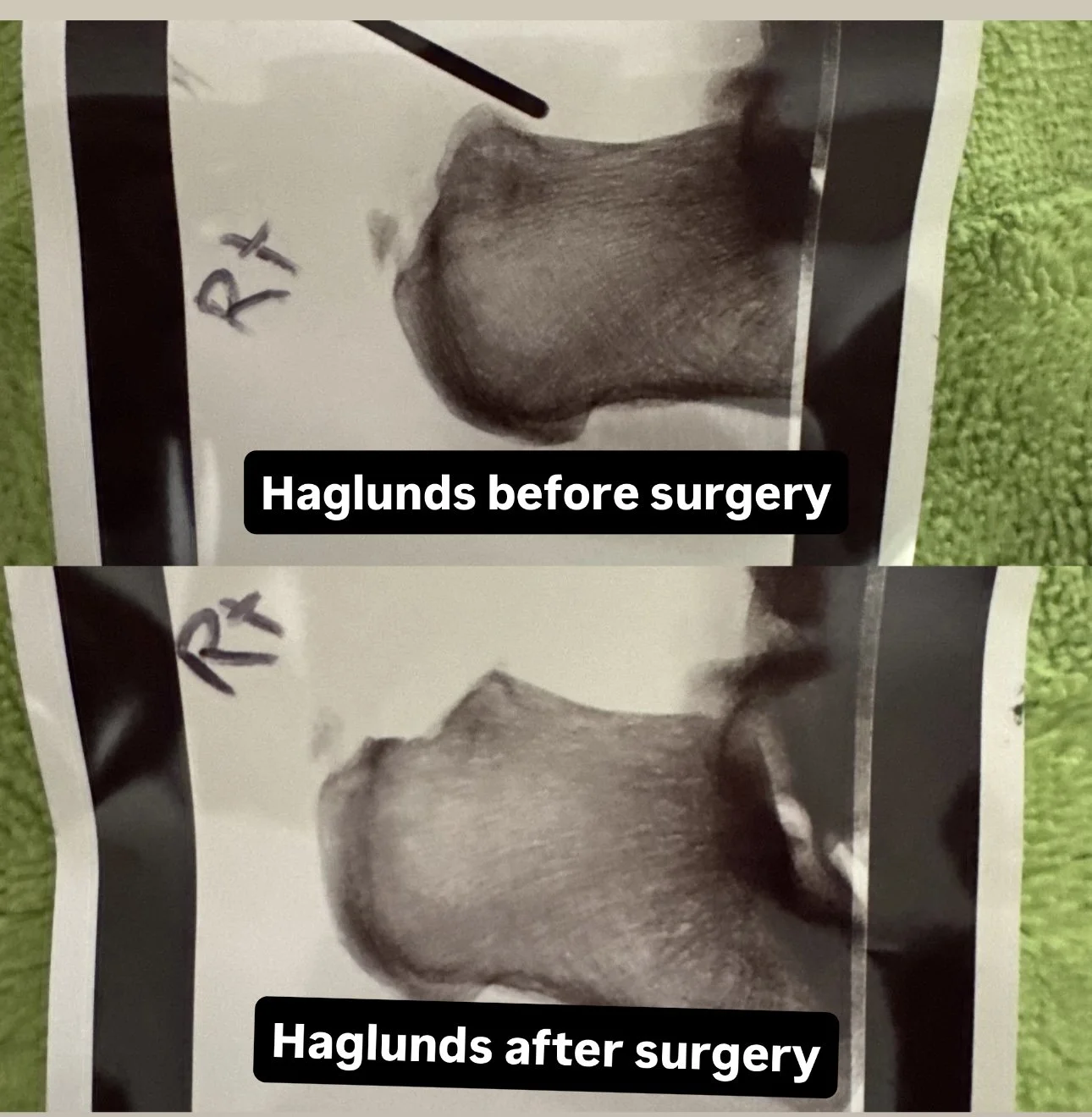
What began as tight Achilles from a lifetime of insufficient stretching, may have led to the incremental growth of my calcaneal tuberosities, the posterior side of both of my heel bones. It’s the old Nature vs Nurture debate. Did chronically tight Achilles stress the bone and force an abnormal protrusion? Was there a degree of genetic predisposition? Perhaps a little of both?
Starting around 2012, I’d begun experiencing pain in the Achilles area. Over the years, I’d met with an athletic trainer, primary care physicians, physical therapists, and finally, an orthopedic surgeon. It wasn’t until meeting with the orthopedist that I had some answers. From tendonitis and tendinopathy, to retrocalcaneal bursitis, nobody had told me the origin of the injury, only the consequences of not dealing with the underlying issue - Haglund’s Deformity. Talk about a name for a bone spur!
When in a seated position, some muscles elongate, like our gluteal and quadricep muscles, while others shorten, like our hip flexors and calf muscles. Upon standing, ramifications from prolonged sitting can be felt, as in my case, the shortened calf muscles elongate, tugging on the Achilles, pressing into the heel. Applying additional tension through contraction to begin walking and the tension within the Achilles presses further into the bone formation, increasing pain. Advance from walking to running and the pressure amplifies. Coupled with a nonexistent relationship with stretching, and over the years, the gentle tug on the calcaneus from the tight calf muscles, and thus, the tight Achilles, stressed the bone to the point of adaptation and growth. Day after day, year after year, X-ray and MRI evidence showed slow, progressive growth of the heel bone, and the writing was on the wall. At this point, no amount of stretching or strengthening, physical therapy or new age medicine was going to fix the continued bone deposits on the back of the heel. The cessation of running or surgery were my only two options.
In May 2025, I ran into Matt, the brother of a well-known high school coach in the Portland community, both of whom were very talented high school and collegiate runners. From an outlook at Hayward Field, I could see Matt talking below with a fellow coach. Matt happened to be wearing two post-surgery removable boots, and having a sense that we had both experienced the same thing, I approached him with one question: “Haglund’s?” Matt immediately replied, “You are the first person to guess it right on the first try. How did you know.” From there, Matt shared his Haglund’s experience with me, and more importantly, his physician.
I met with Dr. Lyle Jackson of Slocum Orthopedics in mid-July, and right off the bat, was greeted with a confident, yet calming presence. Dr. Jackson provided a simple surgical approach to remedy my Haglund’s issue. Surgery could have been scheduled within days, but this provided a dilemma of sorts - have the surgery in early August and miss running the Disneyland Halloween Half Marathon with my daughter in early September, or run the half then have the surgery two days later.
Disney 1, Surgery 0.
Dr. Jackson assured me that I would walk out of the building post-surgery. Matt had told me the same thing, and while I don’t recall much in the hours that followed the surgery courtesy of modern medicine, I was surprised to be putting one foot in front of the other hours after surgery. No pain, no meds.
Aside from a sore throat from the endotracheal tube that supplied the anesthesia during surgery, the day after surgery was day one of recovery. I was able to balance myself and ride my bike to take Boston, our eager golden retriever, to the park for some play. Aside from an Aspirin, day two was medicine free, and to my surprise, still no pain.
Per the generosity of a few individuals, I was provided machines that ran cold water through pads that wrapped around my ankles intended to reduce swelling. Because of the post-op gauze wrapped around my ankle, not much cooling took place, and I presume, any swelling that was present, wasn’t reduced - hard to tell with the gauze and bandage wrappings. Elevating my feet was the only remedy that I could follow in an effort to reduce inflammation.
During the icing efforts, I began toying around with ankle rotations to feel out any limitations or pain from the surgery. Rotating the ankles left, then right, then small circles, only light tugs from the incisions could be felt. Day after day, I began testing the boundaries of my abilities, ensuring myself that I would not go beyond a 4 on the 0-10 pain scale.
After a week of a mostly sedentary lifestyle, I began riding my bike alongside my running partner for his 60-90 minute runs. I also rode the bike at Whisper practices. Most times I rode my bike while wearing my boots, but there were a few times that I felt the need to bring blood circulation to the ankle, feet, and calves, and I would slip on some shoes, over the bandages of course.
While the absence of daily running has been different, remaining actively engaged in the mental and physical recovery process has staved off potential bouts of self-doubt or anxiety. My wife says that I am a doctors worst patient, but I like to think of my current actions as being assertive in my own recovery. Devoting my life to health an fitness, having degrees in health-centered fields, and being fortunate to have really smart friends who are physical therapists, have played key roles in my recovery, albeit only 16 days post-op at this time.
Implements to the right of the boots and medicine ball include 4” and 12” plyo boxes, a Bosu Ball, a Yoga mat, and resistance bands.
THE PSYCHOLOGY OF INJURY & RETURN TO PLAY
My experience with a chronic injury has been handled much different than had I experienced blunt force trauma. I knew surgery was coming, so I was able to mentally process the absence of running. Any experiences within the stages of grief had been dealt with for years, and Acceptance, the final phase, was made when I finally met with Dr. Jackson two months ago in July.
DEPRESSION
The fourth stage of grief is depression, and while it was never on the table in my experience, I can imagine how it could have been had the injury been unexpected, or worse, had the injury or surgery left me without running for the rest of my life. Depression is a normal part of healing and part of the ebbs and flows of life. The key is not holding onto depression for extended lengths of time, and when experiencing depression, using the right tools at our disposal to learn to dance with depression. My repertoire of tools has usually been one thing - exercise.
Beyond the dopamine rush one receives throughout and at the end of an exercise bout, the controlled actions within an exercise setting transfer well into the rest of ones daily activities. Specifically with resistance training, controlling weights, taking them through ranges of motions, provides a sense of control outside of the weight room, whether realized or not. The combined physiological perks, like heightened mood and a greater sense of control, along with being physically stronger and having increased capabilities, and you can understand the role resistance training plays in ones emotional states.
The other three stages of grief, Denial, Anger, and Bargaining, had been worked through regularly since the beginning, and often while on runs. Aiming to work through the pain, telling myself I’ll ice and stretch later if I can get through a run, pushing through the agony of the warm-up. These were all parts of the inner dialogue through it all.
GOALS
My eyes are on the prize. Many prizes in fact. Upon returning to running, I’ll line up for a marathon in an effort to qualify for New York, and if I am fortunate, Berlin. I’d like to also see if a sub-5 mile at 51 years of age is attainable. Sub 2:30 800m, sub-20 5k, sub-40 10k. These are all lofty goals, but if all goes well, why not?
Self-PT has me playing around the edges of pain. I have yet to go beyond 4 on the 0-10 scale, deciding to focus on sustaining ranges of motions in the ankle joint, balance, and general lower body strength. 3-4 sets of 10-20 repetitions provide the stimulus needed to attain the recovery objective. The exercises are familiar, as I have been doing them, and teaching them, for many years before the surgery. For now, while the wound is still fresh, I am staying in the comfort zone, merely trying to adhere to the goals. Any modifications from one workout to the next are efforts in creating a new stimulus, and also to keep things interesting. Here are a few ways exercises were modified during week two of recovery:
Basic squats on the ground to basic squats on a Bosu, performing the same number of sets and reps.
Toe-taps began on a 4” box, then a weight plate was placed beneath the box to add height, in turn increasing the depth of the single-legged squat (toe-tap), which increases joint angles in the standing hip and ankle.
Increase band weight (thickness) when performing calf extensions.
Seeking deeper ranges of motion in the medicine ball teeter exercise.
ALL THE SELF’s
Self-talk, self-belief, self-worth, self-confidence, they have all played a role in my running experience, and now recovery. While the self-negative stuff is easy to let in, the door shuts upon its arrival, and the focus shifts to process and production.
BREATHING AND VISUALIZATION
Both frequent tools in the world of athletics, breathing exercises activates the parasympathetic nervous system, calming the body and increasing focus. Similar to resistance training in that controlling the weights is a metaphor for controlling life outside of the gym, controlled breathing and belly breathing calms nerves and relaxes muscles. Once one is relaxed, the focus can shift toward the task - recovery.
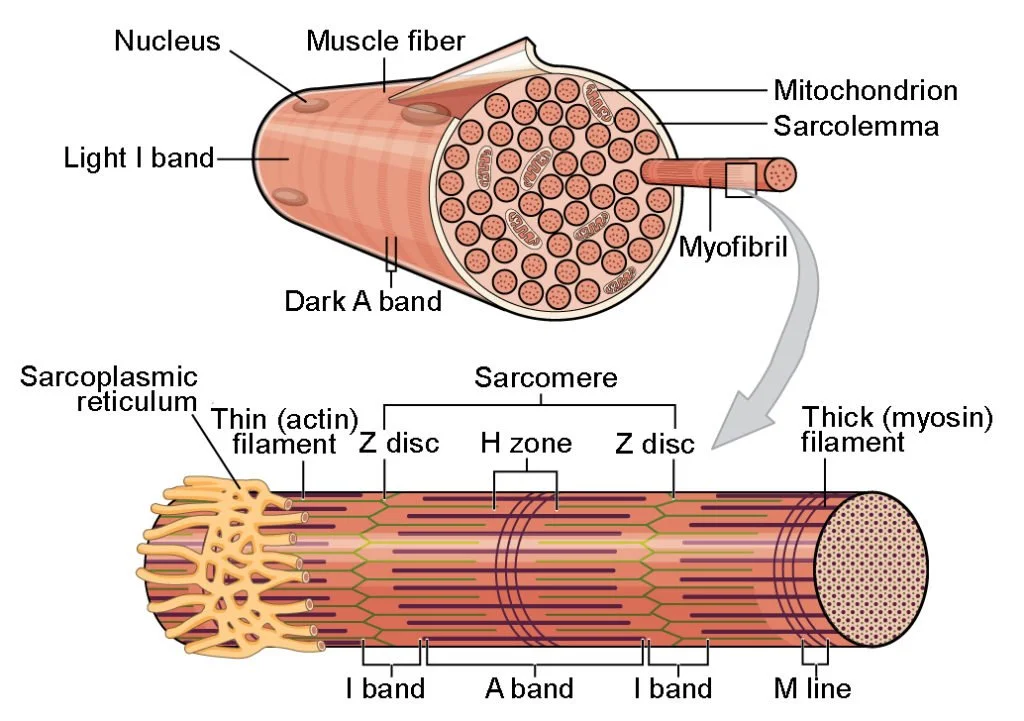
Think of a muscle fiber as a spaghetti noodle touching two walls. When the noodle shortens, it brings the walls together. Because the noodle is shortening, the contents within the noodle overlap, thickening the noodle. Similarly, when contracting a muscle, the muscle fiber shortens and thickens, creating a belly or bulking of the muscle, and the bones come together - think of flexing a biceps muscle, how the radius and ulna bones are brought closer to the humerus, shortening and enlarging the (belly of the) muscle. This pumping action of each repetition brings nutrients and healing to the working muscles (and tendons, ligaments, and bone/joint), and thus, with each repetition, the injury is healing. Whether it takes a week to recover from a strain, or years to recover from sciatica, there is healing when engaging in an appropriately dosed bout of exercise. Seeing these actions through the minds eye is visualization, an integral part in keeping the mind busy during recovery and progress.
COMMUNITY
Who are your peeps?
This is a phase that is easy to allow negative self-talk or self-doubt to creep in. Thinking you are alone, that nobody wants to be alongside an injured athlete, is low hanging fruit in the world of injury. Understanding that these comments are self-made and not reality, and that ultimately, sustaining contact with your little community is part of the healing process. Whether it’s an active role, like riding a bike alongside your running partner(s), or passive, like being a water boy/girl, there is always a place for you - just get there and stay involved! The emotional feel-goods will lift your spirits, and also, promote healing.